Five Common Healthcare Provider Fraud Schemes And How Your Health Insurance Organization Can Prevent Payouts
Healthcare insurance fraud is big business. As much as 10% of annual healthcare expenditures, or $230 billion, are fraudulent. And that’s just what’s been detected. This is costing even the smaller insurers tens of millions of dollars in fake claims payouts. But larger institutions may be on the hook for tens of billions.
Here are five common healthcare provider frauds and how your organization can detect and stop them before costly fraudulent claims are paid out.
BILLING FOR UNNECESSARY OR SERVICES NEVER PERFORMED
Nearly half of all healthcare provider fraud occurs as unnecessary, or non-performed services and procedures.
FALSIFYING CLAIMS OR DIAGNOSES
Up to 25% of all health insurance fraud comes from falsified claims and diagnoses.
ILLEGAL REFERRALS OR KICKBACKS
While it is illegal for a provider to participate in kickbacks, this practice has been known to increase provider profitability by up to 20%.
OVERPRESCRIBING, UNNESESSARY PRESCRIBING
Nearly 11% of all healthcare insurance frauds involve physicians or clinicians over-prescribing or unnecessarily prescribing medications. Often addictive pain-killers with a high street value.
UPCODING AND OVERBILLING
Upcoding is the act of submitting claims for procedures that are more expensive than the actual procedures performed.
Sources:
https://www.bcbsm.com/health-care-fraud/fraud-statistics.html
https://healthpayerintelligence.com/news/top-5-most-common-healthcare-provider-fraud-activities
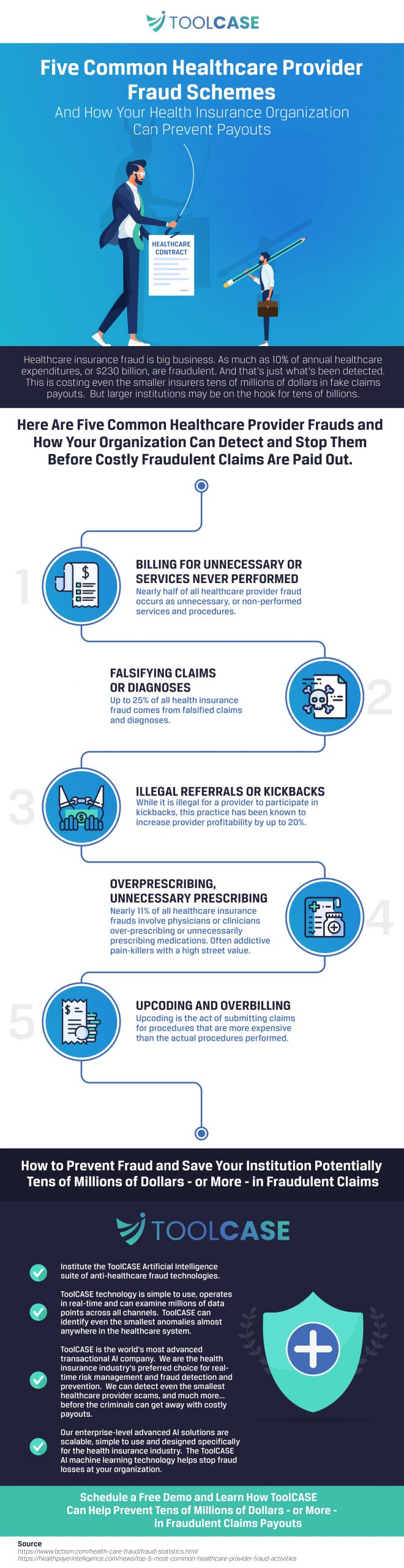
How to Prevent Fraud and Save Your Institution Potentially Tens of Millions of Dollars – or More – in Fraudulent Claims
Institute the ToolCASE Artificial Intelligence suite of anti-healthcare fraud technologies.
ToolCASE technology is simple to use, operates in real-time and can examine millions of data points across all channels. ToolCASE can identify even the smallest anomalies almost anywhere in the healthcare system.
ToolCASE is the world’s most advanced transactional AI company. We are the health insurance industry’s preferred choice for real-time risk management and fraud detection and prevention. We can detect even the smallest healthcare provider scams, and much more… before the criminals can get away with costly payouts.
Our enterprise-level advanced AI solutions are scalable, simple to use and designed specifically for the health insurance industry. The ToolCASE AI machine learning technology helps stop fraud losses at your organization.



